
An Overview of Autism and Aging
Navigating Challenges and Embracing Identity at 50+
~ made by Autism-101.com ~
Jeff Owens - contact[AT]autism-101.com
What Is Autism?
- Autism is a neurological and developmental difference
- It is naturally occurring
- It is not a disease 😷
- It can’t be cured
- It has always existed
Autistic People Differ
“If you have met one autistic person
you have met one autistic person.” [1]
— Dr. Stephen Shore (autism advocate)

Why Are We Talking About This Now?
The Timeline of Invisibility
Why didn’t they get diagnosed 40 years ago?

- 1943-1944: Kanner & Asperger define the condition (mostly in children).
- 1980 (DSM-III): “Infantile Autism” enters the DSM. Strict criteria.
- 1994 (DSM-IV): Asperger’s Syndrome added. The beginning of broader recognition.
- 2013 (DSM-5): ASD becomes a spectrum; allows for adult diagnosis more easily.
“We aren’t part of an epidemic.
We are part of an awakening.”
— Autism-101
Who Are "Older Autistic Adults"?
Today, we are focusing generally on those 50+, but specifically two groups:
- Diagnosed early: now aging.
- "Lost Generation": diagnosed late in life, or still undiagnosed.
Why Were They Missed?
- Diagnostic criteria historically focused on young, white males with high support needs.
- "Masking" or "Camouflaging" to survive education and employment.
- Traits attributed to other things: "quirky," "shy," "difficult," or misdiagnosed with personality disorders/anxiety.
What Triggers a Late Diagnosis?
Often, a life event drastically alters the person's capacity to cope:
- Burnout: Decades of masking finally depletes energy reserves.
- Hormonal Shifts: Perimenopause and menopause can intensify sensory/executive function struggles.
- Major Transitions: Retirement, becoming an empty nester, or loss of a spouse removes stabilizing routines.
- The "Genetic Mirror": Seeing their own traits while their child or grandchild is being assessed.
The Diagnostic Journey
As detailed in books like Lost & Now Found [6] , diagnosis is complex:
Relief & Validation
"I'm not broken; I'm Autistic. There is a name for this."
Grief & Anger
Mourning lost opportunities and decades of struggle without support.
Re-evaluation
Reviewing one's entire life history through a new lens.
Case Study: "Susan" (Age 64)
- Background: Retired librarian. Always called "shy" and "rigid."
- The Trigger: Husband passed away 2 years ago. The loss of his support (handling bills, driving, social buffer) caused a collapse.
- The Misdiagnosis: Diagnosed with Treatment-Resistant Depression and Early Onset Dementia due to "confusion" (which was actually brain fog and burnout).
- The Realization: Read a memoir by an autistic woman and recognized herself.
Sensory Differences
“Processing everyday sensory information can be difficult for autistic people. Any of their senses may be over- or under-sensitive, or both, at different times.” [7]
— NAS
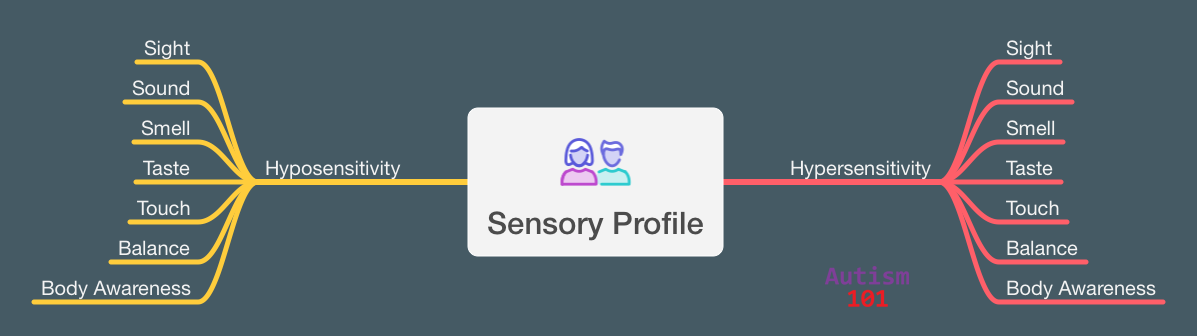
Sensory Profiles
- Unique to individual
- Hyposensitive, hypersensitive, or both
- Can change day to day
- Are well outside the normal ranges
- Impacts what we like to do
Do Sensory Issues “Mellow” With Age?
Short Answer: No. They often become harder to manage.
- Older autistic adults report lower ability to “cope” with sensory input. The energy used to “mask” or “push through” in their 30s is gone.[8]
- Age-related hearing/vision loss increases cognitive load. The brain works harder to interpret data, leading to faster overload.[8]
- After age 40, the autistic nervous system may regulate stress less efficiently, making sensory triggers feel more physically painful.[8]
The “Double Whammy”
Aging and Autism interact bidirectionally:
- Aging processes (cognitive slowing, physical decline) can exacerbate autistic traits (sensory sensitivity, executive dysfunction).
- A lifetime of autistic stress (masking, sensory overload) may accelerate certain aging processes (health outcomes).
Key Concept: Reduced physiological and cognitive "bandwidth" to cope with stressors.
Healthcare Barriers
- Communication Mismatches: Difficulty describing pain accurately; doctors misinterpreting flat affect or direct/blunt communication as non-compliance.
- Sensory Overload in Clinics: Bright lights, waiting rooms, and physical exams can lead to care avoidance.
- Co-occurring Conditions: Higher rates of anxiety, depression, GI issues, and sleep disorders often complicate geriatric care.
Sensory and Cognitive Shifts
- Sensory: Natural age-related hearing/vision loss combined with autistic sensory processing differences can be overwhelming and disorienting.
- Executive Function: Aging impacts working memory and processing speed. For an autistic brain already working hard to organize, this can lead to significant functional decline quickly.
- Burnout Recovery: Bouncing back from sensory or social overload takes significantly longer at 60 than at 30.
Shrinking Support Networks
- Loss of “Buffers”: Many older autistics relied heavily on parents or a spouse to navigate the social world. Losing them is catastrophic.
- The “Group Home” Fear: Intense fear of losing independence and ending up in communal senior living, which is rarely sensory-friendly.
- Financial Vulnerability: Due to lifetime underemployment (common in the lost generation), financial resources for aging may be scarce.
Co-occuring Conditions
- Will likely have other issues
- Ex. ADHD may occur in 40% to 70% of autistic people [9]

The "Autistic Advantage" in Aging
It isn't all negative. Many older autistic adults possess unique resilience factors:
- Solitude as Strength: Often better equipped to handle alone time than neurotypical peers.
- Passionate Interests: "Special Interests" provide deep engagement, cognitive protection, and joy in retirement.
- Non-Conformity: Less pressure to keep up with societal expectations of "how to act" at 70.
Supporting Older Autistic Adults
- Believe them: If they say they are autistic late in life, validate it. Do not demand a difficult-to-obtain formal diagnosis to provide support.
- Sensory Audits: Evaluate living spaces for sensory triggers (lighting, humming noises, textures).
- Clear Communication: In healthcare and legal planning, use literal, clear language. Allow extra processing time.
- Redefining "Social": Respect the need for solitude. Connection doesn't have to mean group activities in a noisy senior center.
Moving Forward: Unmasking
Unmasking is crucial for healthy aging.
- Preserving energy by stopping the performance of "neurotypicality."
- Allowing stimming and sensory aids (headphones, sunglasses) without shame.
- Connecting with the autistic community (often online) to share lived experiences.
The Future of Aging
We need a paradigm shift in geriatric care.
- Neurodiversity-affirming training for geriatricians and care home staff.
- More research focused on the quality of life for the 60+ autistic population.
- "Nothing about us without us" extends to our elders.
Thank you for listening.
contact[AT]autism-101.com ~ https://autism-101.com